Two articles: Kids don't need no stinkin' vaccinations
Trump and Bobby Jr. seem intent on bringing back infectious diseases for reasons unknown
Stephanie Soucheray, MA and Liz Szabo, MA
Federal officials today announced an unprecedented overhaul of the US childhood immunization schedule, paring the number of universally recommended immunizations from 17 to 11.The new vaccination policy,
which takes effect immediately, is modeled after the schedule used by
Denmark. Although the Centers for Disease Control and Prevention (CDC)
will continue to recommend 11 shots for all children, six others will be
recommended only for children deemed to be at high risk of infection, said the
agency’s acting director, Jim O’Neill.
A third group of vaccines will be available through “shared
clinical decision-making” with medical providers.
Public health experts immediately decried the
change. Experts said there’s no reason to change a system that has prevented 1.1 million
deaths over the past 30 years.
“Abandoning the U.S. evidence-based process is a dangerous
and potentially deadly decision for Americans,” said Jason M. Goldman, MD,
president of the American College of Physicians. “The evidence is clear that
vaccines prevent deaths, hospitalizations, and spread of disease.”
New schedule recommends shots against 11 diseases, down from 17
The CDC will continue to recommend vaccines against 11
diseases for all children, including measles, mumps, rubella, polio, pertussis,
tetanus, diphtheria, Haemophilus influenzae type B (Hib),
pneumococcal disease, human papillomavirus (HPV), and varicella (chickenpox).
The CDC is recommending six shots for “high-risk groups,”
including vaccines that protect against respiratory syncytial virus (RSV),
hepatitis A, hepatitis B, dengue and two vaccines targeting bacterial
meningitis (MenACWY and MenB). Dengue vaccines have always been targeted only
to a relatively small number of children in specific circumstances.
The vaccines recommended for shared clinical decision-making
are for rotavirus, COVID-19, influenza, meningococcal disease, hepatitis A, and
hepatitis B.
In another important change, the CDC is now recommending
only one dose of HPV vaccine. Until today, the CDC recommended two or three HPV
vaccines, depending on the age at which children receive their first shot. EDITOR'S NOTE: HPV vaccine has been shown to be remarkably effective in preventing cervical and other cancers.
The new policy emphasizes that all vaccines recommended for
any of the three categories will remain covered by insurance.
Health and Human Services (HHS) Secretary Robert F. Kennedy
Jr. has long claimed that US children receive “too many” vaccines. This announcement addresses his long-held wish to reduce the number of immunizations
that children receive.
It also fulfills a directive issued by President Donald
Trump last month calling for HHS to align the US vaccination schedule with that
of Denmark and other countries that recommend fewer vaccines. The CDC said the
changes followed an assessment of 20 developed nations, most of which have
national health care systems that provide free health care to their citizens
from birth to death. EDITOR'S NOTE: This is the same Denmark the US is threatening with war over Greenland.
Experts say changes are radical, dangerous
“This is a very dark day for children and for their parents
and for our country generally,” said Jesse Goodman, MD, MPH, a professor of
medicine and infectious diseases at Georgetown University, who spoke at a press
conference of vaccine experts following the announcement.
Goodman compared the announcement to a “torpedo” blowing up
vaccination policy. “There will be more diseases, more infection, more
hospitalization,” said Goodman, a former Food and Drug Administration (FDA)
chief scientist and former director of the agency’s center for biologics
evaluation and research.
Officials with the American Academy of Pediatrics (AAP), which has not changed its childhood vaccination recommendations, also oppose the new schedule. Many pediatricians and family doctors tell CIDRAP News that they will continue to follow AAP’s guidance, rather than that of the CDC.
“I’m not sure why they want to bring the diseases back but
that’s their goal,” said Sean O’ Leary, MD, who chairs the AAP’s infectious
disease committee, during a separate press conference held after the
announcement. “With RSV we’ve already seen population-level impact. Why do they
want more hospitalizations? Hepatitis A is a miserable disease, and it’s
particularly bad as children age.”
Michael Osterholm, MPH, PhD, of the Vaccine Integrity
Project and the director of the University of Minnesota's Center for Infectious
Disease Research and Policy (CIDRAP), which publishes CIDRAP News, called
today’s announcement a radical move.
“Eliminating vital US childhood vaccine recommendations
without public discussion or transparent review of the data the decision was
based on is a radical and dangerous decision,” Osterholm said. “This wildly
irresponsible decision will put lives at risk.”
Eying a return of vaccine-preventable diseases
The changes to the childhood immunization schedule come as
more US children are dying from vaccine-preventable diseases, which have
returned as immunization rates have declined.
Two Texas children died from measles last year in an
outbreak that has reached more than 2,000 cases and shows no sign of stopping.
Thirteen people died from pertussis,
also known as whooping cough, which infected nearly 28,000 Americans last year.
The United States also recorded
at least 288 flu deaths in children last year, the highest number
for a non-pandemic flu season. Several children already have died of flu this
year, in what is predicted to be a severe influenza season.
“Given the intensity of the current flu season and this
guidance from the political appointees at HHS, it seems likely we will see even
more deaths this year,” Kevin Ault, MD, a professor of obstetrics and
gynecology at the Western Michigan University Homer Stryker School of Medicine.
“Making these changes amid ongoing outbreaks of
vaccine-preventable diseases shows a disregard for the real confusion families
already face,” Infectious Diseases Society of America President Ronald Nahass,
MD, said in a statement.
During the AAP press conference, O’Leary said the emphasis
on shared clinical decision-making will only further confuse both parents and
doctors.
“The fact is, pediatricians already do this all day, every
day,” he said. “It just makes things more confusing for parents and clinicians.
So when the evidence is clear that the benefits outweigh the risks, the
guidance should be clear, not confusing as what has now happened today.”
Changes likely to be challenged in court
The Trump administration has circumvented the usual process
for updating vaccine schedules, which normally involves input from scientific
experts, public health leaders, and other stakeholders, Ault said.
An 80-year-old law called the Administrative Procedures
Act requires
that federal officials follow an open, deliberative process when
issuing rules and regulations. The law forbids federal officials from making
decisions that are “arbitrary and capricious.”
The AAP already filed a lawsuit against Kennedy in July, claiming that he violated the APA when he issued a directive removing the COVID-19 vaccine from the CDC immunization schedule for children and pregnant women.
For vaccines, that process typically includes public
meetings by ACIP, which makes vaccine recommendations which the CDC director
can accept or reject. These meetings are announced in advance, with opportunity
for written comments ahead of the meeting, as well as time for the public to
speak during the meeting.
“For decades, changes in the American vaccine have been
discussed in public meetings at the CDC with expert review of the available
evidence,” said Ault, a former member of ACIP. “The new guidelines are not
supported by data, and there was no input from stakeholder groups like the
American Academy of Pediatrics and the American Academy of Family
Physicians.”
“The goal of this administration is to make vaccines
optional,” said Paul Offit, MD, an infectious disease specialist at Children’s
Hospital of Philadelphia. “I think that’s where we’ve been moving.”
Vaccine vandal is taking us back to the 1950s
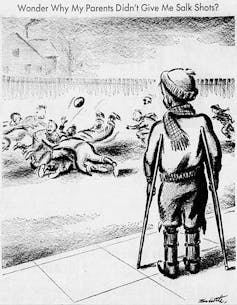 |
| This editorial cartoon commenting on the polio vaccine won the Pulitzer Prize in 1956. Tom Little via Wikimedia Commons |
The Trump administration’s overhauling of the decades-old childhood vaccination schedule, announced by federal health officials on Jan. 5, 2026, has raised alarm among public health experts and pediatricians.
The U.S. childhood immunization schedule, the grid of colored bars pediatricians share with parents, recommends a set of vaccines given from birth through adolescence to prevent a range of serious infections. The basic structure has been in place since 1995, when federal health officials and medical organizations first issued a unified national standard, though new vaccines have been added regularly as science advanced.
That schedule is now being dismantled.
In all, the sweeping change reduces the universally recommended childhood vaccines from 17 to 11. It moves vaccines against rotavirus, influenza, hepatitis A, hepatitis B and meningococcal disease from routine recommendations to “shared clinical decision-making,” a category that shifts responsibility for initiating vaccination from the health care system to individual families.
Health and Human Services Secretary Robert F. Kennedy Jr., who has cast doubt on vaccine safety for decades, justified these changes by citing a 33-page assessment comparing the U.S. schedule to Denmark’s.
But the two countries differ in important ways. Denmark has 6 million people, universal health care and a national registry that tracks every patient. In contrast, the U.S. has 330 million people, 27 million uninsured and a system where millions move between providers.
These changes follow the CDC’s decision in December 2025 to drop a long-held recommendation that all newborns be vaccinated against hepatitis B, despite no new evidence that questions the vaccine’s long-standing safety record.
I’m an infectious disease physician who treats vaccine-preventable diseases and reviews the clinical trial evidence behind immunization recommendations. The vaccine schedule wasn’t designed in a single stroke. It was built gradually over decades, shaped by disease outbreaks, technological breakthroughs and hard-won lessons about reducing childhood illness and death.
The early years
For the first half of the 20th century, most states required that students be vaccinated against smallpox to enter the public school system. But there was no unified national schedule. The combination vaccine against diphtheria, tetanus and pertussis, known as the DTP vaccine, emerged in 1948, and the Salk polio vaccine arrived in 1955, but recommendations for when and how to give them varied by state, by physician and even by neighborhood.
The federal government stepped in after tragedy struck. In 1955, a manufacturing failure at Cutter Laboratories in Berkeley, California, produced batches of polio vaccine containing live virus, causing paralysis in dozens of children. The incident made clear that vaccination couldn’t remain a patchwork affair. It required federal oversight.
In 1964, the U.S. surgeon general established the Advisory Committee on Immunization Practices, or ACIP, to provide expert guidance and recommendations to the CDC on vaccine use. For the first time, a single body would evaluate the evidence and issue national recommendations.
New viral vaccines
Through the 1960s, vaccines against measles (1963), mumps (1967) and rubella (1969) were licensed and eventually combined into what’s known as the MMR shot in 1971. Each addition followed a similar pattern: a disease that killed or disabled thousands of children annually, a vaccine that proved safe and effective in trials, and a recommendation that transformed a seemingly inevitable childhood illness into something preventable.
The rubella vaccine went beyond protecting the children who received it. Rubella, also called German measles, is mild in children but devastating to fetuses, causing deafness, heart defects and intellectual disabilities when pregnant women are infected.
A rubella epidemic in 1964 and 1965 drove this point home: 12.5 million infections and 20,000 cases of congenital rubella syndrome left thousands of children deaf or blind. Vaccinating children also helped protect pregnant women by curbing the spread of infection. By 2015, rubella had been eliminated from the Americas.
Hepatitis B and the safety net
In 1991, the CDC added hepatitis B vaccination at birth to the schedule. Before then, around 18,000 children every year contracted the virus before their 10th birthday.
Many parents wonder why newborns need this vaccine. The answer lies in biology and the limitations of screening.
An adult who contracts hepatitis B has a 95% chance of clearing the virus. An infant infected in the first months of life has a 90% chance of developing chronic infection, and 1 in 4 will eventually die from liver failure or cancer. Infants can acquire the virus from their mothers during birth, from infected household members or through casual contact in child care settings. The virus survives on surfaces for days and is highly contagious.
Early strategies that targeted only high-risk groups failed because screening missed too many infected mothers. Even today, roughly 12% to 18% of pregnant women in the U.S. are never screened for hepatitis B. Until ACIP dropped the recommendation in early December 2025, a first dose of this vaccine at birth served as a safety net, protecting all infants regardless of whether their mothers’ infection status was accurately known.
This safety net worked: Hepatitis B infections in American children fell by 99%.
A unified standard
For decades, different medical organizations issued their own, sometimes conflicting, recommendations. In 1995, ACIP, the American Academy of Pediatrics and the American Academy of Family Physicians jointly released the first unified childhood immunization schedule, the ancestor of today’s familiar grid. For the first time, parents and physicians had a single national standard.
The schedule continued to evolve. ACIP recommended vaccinations for chickenpox in 1996; rotavirus in 2006, replacing an earlier version withdrawn after safety monitoring detected a rare side effect; and HPV, also in 2006.
Each addition followed the same rigorous process: evidence review, risk-benefit analysis and a public vote by the advisory committee.
More vaccines, less burden
Vaccine skeptics, including Kennedy, often claim erroneously that children’s immune systems are overloaded because the number of vaccines they receive has increased. This argument is routinely marshaled to argue for a reduced childhood vaccination schedule.
One fact often surprises parents: Despite the increase in recommended vaccines, the number of immune-stimulating molecules in those vaccines, called antigens, has dropped dramatically since the 1980s, which means they are less demanding on a child’s immune system.
The whole-cell pertussis vaccine used in the 1980s alone contained roughly 3,000 antigens. Today’s entire schedule contains fewer than 160 antigens, thanks to advances in vaccine technology that allow precise targeting of only the components needed for protection.
What lies ahead
For decades, ACIP recommended changes to the childhood schedule only when new evidence or clear shifts in disease risk demanded it. The Jan. 5 announcement represents a fundamental break from that norm: Multiple vaccines moved out of routine recommendations simultaneously, justified not by new safety data but by comparison to a country with a fundamentally different health care system.
Kennedy accomplished this by filling positions involved in vaccine safety with political appointees. His hand-picked ACIP is stacked with members with a history of anti-vaccine views. The authors of the assessment justifying the change, senior officials at the Food and Drug Administration and at HHS, are both long-time critics of the existing vaccine schedule. The acting CDC director who signed the decision memo is an investor with no clinical or scientific background.
The practical effect will be felt in clinics across the country. Routine recommendations trigger automatic prompts in medical records and enable nurses to vaccinate under standing orders. “Shared clinical decision-making” requires a physician to be involved in every vaccination decision, creating bottlenecks that will inevitably reduce uptake, particularly for the more than 100 million Americans who lack regular access to primary care.
Major medical organizations, including the American Academy of Pediatrics and the American College of Obstetricians and Gynecologists, have said that they will continue recommending the full complement of childhood vaccines. Several states, including California, New York and Illinois, will follow established guidelines rather than the new federal recommendations, creating a patchwork where children’s protection depends on where they live.
Portions of this article originally appeared in a previous article published on Dec. 18, 2025.![]()
Jake Scott, Clinical Associate Professor of Infectious Diseases, Stanford University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
