A pandemic in its own right?
Chris Robinson, University of Florida
 |
| COVID-19 survivors face not only physical symptoms. A large study recently showed that their mental health is affected, too. FG Trade/Getty Images |
Researchers looked at 236,379 British patients diagnosed with COVID-19 over six months, analyzing neurologic and psychiatric complications during that time period.
They compared those individuals to others who had experienced similar respiratory illnesses that were not COVID-19.
They found a significant increase in several medical conditions among the COVID-19 group, including memory loss, nerve disorders, anxiety, depression, substance abuse and insomnia. Additionally, the symptoms were present among all age groups and in patients who were asymptomatic, isolating in home quarantine, and those admitted to hospitals.
The results of this study speak to the seriousness of long-term consequences of COVID-19 infection. Numerous reports of brain fog, post-traumatic stress disorder, heart disease, lung disease and gastrointestinal disease have peppered the media and puzzled scientists over the past 12 months, begging the question: What effect does COVID-19 have on the body long after the acute symptoms have resolved?
I am an assistant professor of neurology and neurosurgery and can’t help but wonder what we have learned from past experience with other viruses. One thing in particular stands out: COVID-19 consequences will be with us for quite some time.
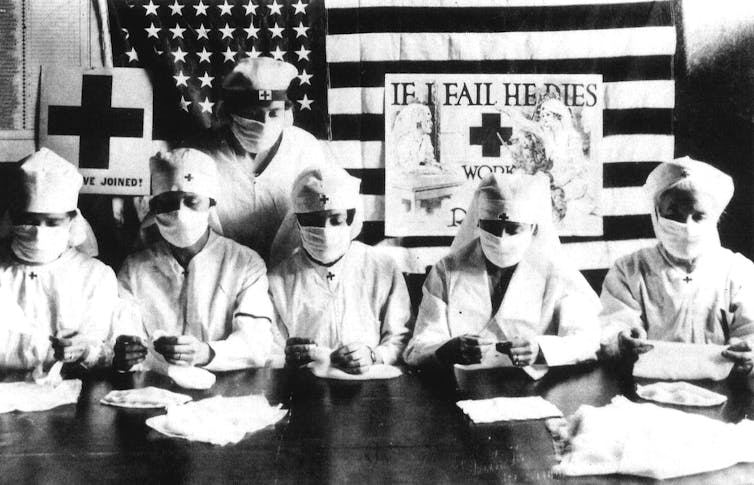 |
| Red Cross volunteers during the 1918 flu pandemic. Apic/Getty Images |
Learning from history
Past virus outbreaks, such as the 1918 flu pandemic and the SARS epidemic of 2003, have provided examples of the challenges to expect with COVID-19. And, the long-term effects of other viral infections help provide insight.
Several other viruses, including a large majority of those that cause common upper and lower respiratory infections, have been shown to produce such chronic symptoms as anxiety, depression, memory problems and fatigue. Experts believe that these symptoms are likely due to long-term effects on the immune system. Viruses trick the body into producing a persistent inflammatory response resistant to treatment.
Myalgic encephalomyelitis, also known as chronic fatigue syndrome, is one such illness. Researchers believe this condition results from continuous activation of the immune system long after the initial infection has resolved.
In contrast to other viral infections, the COVID-19 survivors in the study reported persistent symptoms lasting more than six months, with no significant improvement over time. The abundance of psychiatric symptoms was also notable and likely attributable to both infection and pandemic-related experience.
These findings are leading researchers to hypothesize several mechanisms following acute COVID-19 infection that may lead to long-haul COVID-19. With the known historical context of chronic symptoms following other viruses, doctors and researchers may have a glimpse into the future of COVID-19 with the potential to create therapies to alleviate patients’ persistent symptoms.
 |
| Scott Krakower, a psychiatrist, poses in front of his home on July 8, 2020 in Port Washington on Long Island, N.Y. Krakower is a COVID-19 long-hauler. Johannes Eisele/AFP via Getty Images |
COVID-19 is now known to be a disease that affects all organ systems, including the brain, lungs, heart, kidneys and intestines.
Several theories exist as to the cause of chronic, lingering symptoms. Hypotheses include direct organ damage from the virus, continual activation of the immune system after acute infection and persistent lasting virus particles that find safe harbor within the body.
To date, autopsy studies have not confirmed the presence or overabundance of COVID-19 particles in the brain, making the immune theories the most likely cause of brain dysfunction.
Some recovered COVID-19 patients detail significant improvement or resolution of long symptoms following inoculation with the COVID-19 vaccine. Others report improvement following a short course of steroids. The most plausible explanation for the direct effects of long COVID-19 on the brain are due to its body-wide connections and the fact that COVID-19 is a multi-organ disease.
These findings may point to a direct immune related cause of long COVID-19, though no real answers yet exist to define the true cause and duration of the disease.
The post-COVID-19 world
In February, the National Institutes of Health announced a new initiative to study long COVID-19, now collectively defined as Post-Acute Sequelae of SARS-CoV-2. The NIH created a fund of US$1.15 billion to study this new disease. The aims of the study include the cause of long-term symptoms, the number of people affected by the disease and vulnerabilities leading to long COVID-19.
In my view, public health officials should continue to be open and transparent when discussing the short- and long-term effects of COVID-19. Society as a whole needs the best information possible to understand its effects and resolve the problem.
COVID-19 remains and will continue to be one of the largest socioeconomic problems across the world as we begin to recognize the true long-term impacts of the disease. Both the scientific and research communities should continue to be diligent in the fight long after the acute infections are gone. It appears that the chronic effects of the disease will be with us for some time to come.
[Get facts about coronavirus and the latest research. Sign up for The Conversation’s newsletter.]![]()
Chris Robinson, Assistant Professor of Neurology and Neurosurgery, University of Florida
This article is republished from The Conversation under a Creative Commons license. Read the original article.