The mystery bureaucrats managing your prescription drugs
By Linda L Ujifusa, Esq & J Mark Ryan, MD FACP in UpRiseRI
SHORT ATTENTION SPAN ALERT:
This is a long article. It needs to be. If you can only handle Tweet-length pieces, you should move along now. However, if you live in Rhode Island and take prescription medicines through any insurance plan, including Medicare D, this article discusses issues that directly affect you and also offers suggestions for actions you should take. - Will Collette
SUMMARY:
About
40% of Americans struggle to afford their regular prescription medicines – with
1/3 saying they have skipped filling a prescription one or more times, because
of the cost. COVID-19 has exacerbated the problem by causing job and
health insurance loss and delaying routine care.
Rhode
Island policymakers know skyrocketing prescription drug prices must be better
controlled.
Unfortunately,
they have ignored a key cost driver: Pharmacy Benefit Managers (PBMs).
PBMs
such as CVS Caremark, Express Scripts and OptumRx “manage” prescription drug
benefits on behalf of insurers and siphon off enormous revenues in the complex
non-transparent system that gets drugs from manufacturers to patients.
Other
states are doing a much better job monitoring and controlling PBMs and have
saved consumers and tax payers hundreds of millions of dollars.
Rhode
Island should follow their lead.
To
urge RI policymakers to take action, please sign this petition.
A
fully footnoted version of this article is available to download here.
What
are PBMs?
In
between most patients and healthcare providers are middlemen health insurers
(“payers”) who take money from patients, pay some to healthcare providers, and
keep some for themselves. These multiple payers cause the United States to
spend about twice per capita what other industrialized nations with “single
payer” spend and they get better universal healthcare.
In the middle of payers, patients and pharmacies, there are Pharmacy Benefit Managers (PBMs).
PBMs:
Middlemen for middlemen
PBMs
are for-profit companies that “manage” prescription drug benefits for more than
266 million Americans on behalf of payers, including private
insurers, Medicare Part D drug plans, government employee plans,
large employers, and Medicaid Managed Care Organizations (MCOs).
PBMs
help payers:
- create a list of covered drugs for plans (“a formulary”);
- manage drug utilization by enrollees (e.g., by setting co-pays, prior authorization policies, etc.);
- reimburse pharmacies for providing the enrollee drugs.
This
article will focus on:
- Who are Pharmacy Benefit Managers (PBMs)
- How PBMs Harm Consumers and Taxpayers
- PBM Oversight in Other States
- Potential Roadblocks to RI Reforms
- How RI Can Rein in PBMs
WHO
ARE PHARMACY BENEFIT MANAGERS (PBMS)
PBMs
began in the 1970s as small independent middlemen between insurers and
pharmacies, taking a set fee for processing claims.
Today,
three PBMs control 80% of the market and are part of large vertically
integrated conglomerates that include health insurance companies and pharmacies (including
“specialty
pharmacies”)
- CVSCaremark – 32% market share – parent company: CVS (Aetna)
- Express Scripts – 24% market share – parent company: Cigna
- OptumRx – 21% market share – parent company: UnitedHealth
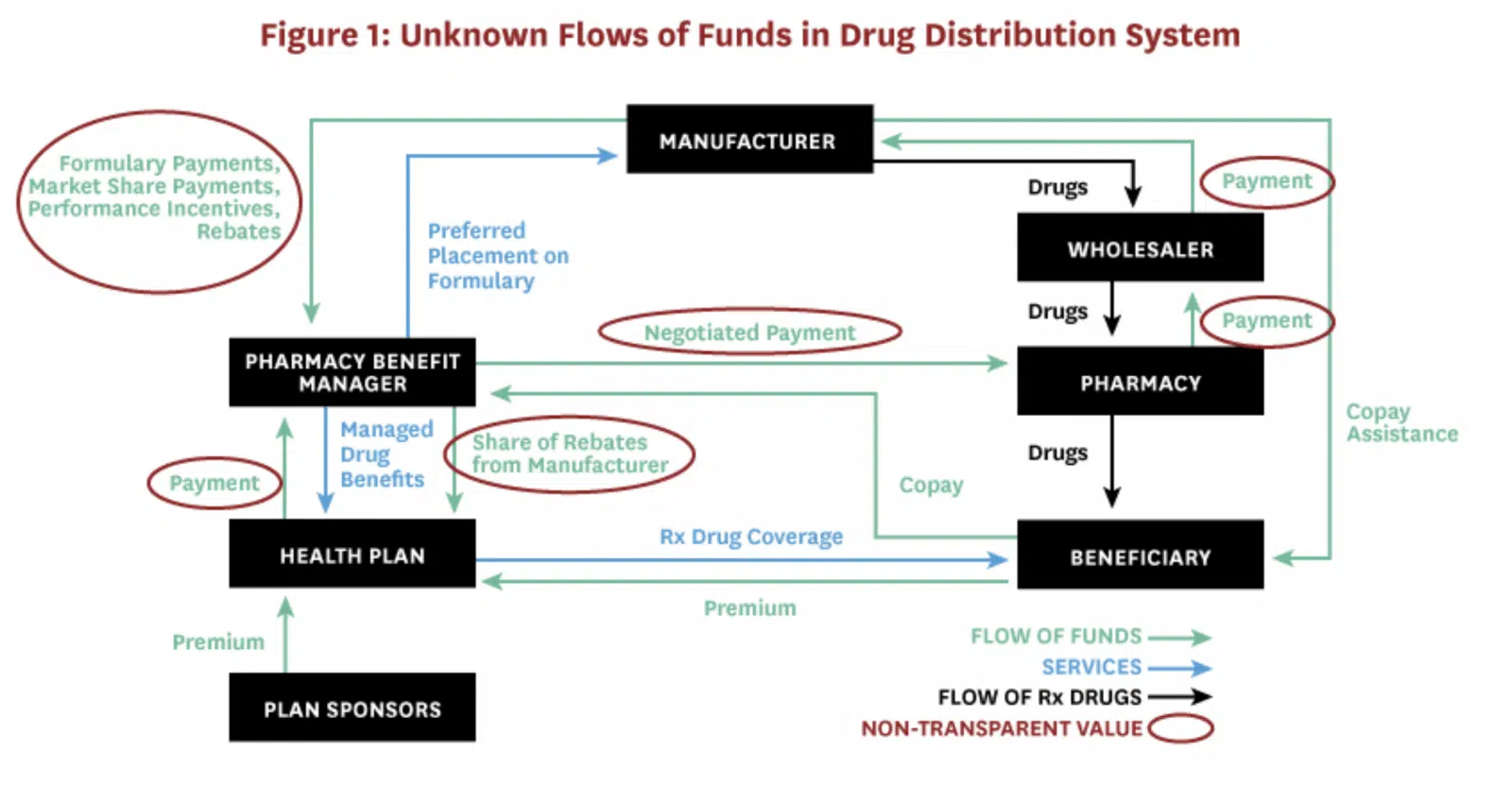
PBMs are also part of a complex non-transparent distribution system that gets drugs from manufacturers to beneficiaries (see Figure 1).
Source: https://healthpolicy.usc.edu/research/state-drug-pricing-transparency-laws-numerous-efforts-most-fall-short/, adapted from, Sood, N., et al., “Flow of Money Through the Pharmaceutical Distribution System,” USC Schaeffer Center for Health Policy white paper.
In
this system, businesses can keep payments and discounts between themselves
confidential, but analyses show that pharmaceutical manufacturers make the most
profits for developing and manufacturing prescription drugs AND:
Revenues
of top PBM conglomerates exceed those of top pharmaceutical manufacturers.
PBM
conglomerates rank 4th (CVS), 5th (UnitedHealth
Group) and 13th (Cigna) on the Fortune 500 list ranking largest
corporations by revenue.
PBMs
drive revenues for their parent companies:
- “CVS Health’s Pharmacy Services (PBM) segment will make 46% of $324 Billion in 2021 revenues for the company and remains key to its revenue growth.”
- In 2019, Cigna’s total revenues more than doubled ($14.3 billion to $38.2 billion) and its Express Scripts Holding Co. unit was the “driving force” behind the $22 billion surge.
- UnitedHealth’s Optum subsidiaries collected more profit in the fourth quarter of 2019 ($3 billion) than United Healthcare insurance ($2.1 billion)
HOW
PBMs HARM CONSUMERS AND TAXPAYERS
1.
PBMs get legal kickbacks (“rebates”) from drug manufacturers for putting
certain drugs on formularies
When
PBMs create a list of covered drugs, they negotiate with drug manufacturers for
legal kickbacks (“rebates”) in exchange for giving certain drugs preferred
placement on formularies (e.g., Tier 1 with no co-pay, etc.).
Kickbacks
are generally illegal under federal law, but PBMs are given a “safe harbor” and
a federal rule making PBM rebates illegal has been delayed.
PBMs
have a conflict of interest developing formularies because they get
more money for shareholders by choosing an expensive drug with a higher rebate
than by choosing the most effective or affordable drug for consumers.
Although
PBMs pass rebates to insurers (who may be their parent companies) and claim
this will result in lower premiums and co-pays, analyses show there is no such
trickle down to consumers.
In
fact, drug manufacturers cover PBM rebates by raising their
list prices for drugs and consumers pay a higher co-pay
because they pay a % of the higher list prices.
At
$143 billion in 2019, it is estimated that rebates added nearly 30 cents per
dollar to the price consumers pay for prescriptions.
2.
PBMs overcharge payers (including state Medicaid) and underpay pharmacies
because they can keep the difference (“spread”) between what they are paid and
how much they reimburse pharmacies
Multiple
states have found PBMs problems related to their keeping the “spread.” An
Ohio audit, for example, found that in one year, “CVS Caremark and
UnitedHealth’s OptumRx PBMs reaped more than $223 million—and made an 8.8%
profit—by overcharging Medicaid managed care plans, underpaying pharmacies,
and pocketing the difference.”
Ohio
found the spread came to $5.70 per prescription across all brand-name and
generic drugs and that Ohio could have gotten the same services for $1.90 per
prescription or less by switching to a fee-based model – where pharmacies are
reimbursed their acquisition cost plus a set administrative fee.
Ohio
ordered managed-care plans in the state to terminate PBM spread pricing
contracts for 2019.
3.
PBMs “claw back” and keep excess consumer co-pays
Consumers
are often unaware they could have paid less if they had NOT used their
insurance (for example, when a co-pay is $10, but the drug price without
insurance is $7).
Although
consumers should be allowed to recover such overpayments, PBMs are the ones who
“claw back” overpayments – and keep them.
A study by
researchers at the University of Southern California Schaeffer Center for
Health Policy & Economics found that because of PBM claw backs, customers
overpaid for their prescriptions 23 percent of the time.
4. PBMs
profit from a federal program (“Section 340B”) meant to help low income
patients
In
1992, Congress enacted Section 340B of the Public Health Service Act mandating
that pharmaceutical manufacturers provide outpatient drugs at significant
discounts to certain “covered entities.” 340B’s original purpose was to
allow a handful of safety-net hospitals that cared for the poor to obtain drugs
at substantially reduced prices.
Changing
federal laws caused the number of entities eligible for 340B discounts to
explode so that today, there are now about 5,000 covered entities and 20,000
affiliated sites, as well as, “30,000 pharmacy locations—half of the entire
United States pharmacy industry – now act[ing] as contract pharmacies for the
hospitals and other healthcare providers that participate in the 340B
program.” 340B discounted drugs make up “more than 8% of the total United
States. drug market and about 16% of the total rebates and discounts that
manufacturers provide.”
This
large, complex and relatively unknown program is detailed here,
but PBM problems generally involve their engaging in “discriminatory reimbursement,”
e.g., offering 340B entities lower reimbursement rates than those offered to
non-340B entities.
Currently,
the federal 340B statute allows PBMs to make significant revenues and not pass
money to those Section 340B intended to help.
5. PBM
conglomerates own retail, mail order and specialty pharmacies and can work
against consumer interests by:
- Setting low reimbursements for their competitors – a cause of local independent pharmacies disappearing.
- Pharmacy Steering – PBMs “steer” customers to pharmacies, including mail order and specialty pharmacies, with whom they are affiliated, e.g., by requiring a higher copay if the patient obtains the drug from a non-affiliated pharmacy.
- Pharmacist gag orders – despite a federal law and a new 2021 Rhode Island law that prohibits PBMs from preventing pharmacists from discussing cheaper options, the consumer still has to ask and may not be told all options.
6.
PBMs can hide profits
Reasons
for the lack of transparency noted in Figure 1 include:
- PBMs keeping their negotiated discounts and rebates confidential – even from a recent federal Senate committee investigating insulin prices.
- PBMs disguising profits, e.g., as “rebate management fees” and “savings.”
- PBMs controlling their own audits, e.g., by having the right to veto auditors, determine frequency of audits, require auditors to sign “Confidentiality Agreements,” etc.
7.
PBM “Utilization Management” can harm patients
PBMs
claim to implement “utilization management” strategies on behalf of payers to
benefit payers AND consumers. These strategies can include:
- “Prior authorization,” which requires patients to get third-party approval prior to getting the medicine prescribed by their healthcare provider.
- “Step therapy,” also known as “fail-first,” “sequencing,” and “tiering,” which requires patients to start with lower-priced medications before being approved for originally prescribed medications.
- “Non-medical drug switching” which forces patients off their current therapies for no reason other than to save money. “Tactics include increasing out-of-pocket costs, moving treatments to higher cost tiers, or terminating coverage of a particular drug.
Unfortunately,
such utilization management can also harm consumers by making providers spend
excessive time on administrative tasks, delaying and discouraging patient care,
and adversely affecting clinical outcomes.
PBM
Oversight in Other States
Rhode
Island has some PBM-related laws and regulations, but other states are more
aggressively investigating and reining in PBMs to better protect consumers and
tax payers.
A
recent Supreme Court case, Rutledge v.
PCMA, supports states taking more actions to regulate PBMs.
Some
actions other states are taking include:
1. Imposing
transparency reporting requirements
27
states with private insurance companies (Managed Care Organizations –
MCOs) managing their Medicaid programs reported they will have transparency
reporting requirements in place in FY 2020. For example:
Texas passed
a 2019 law requiring PBMs to report information to the state and discovered,
“Since 2016, through a complex rebate and price concession process, the PBM
industry in Texas pocketed more than $350 million in revenue, while passing a
mere $16 million in savings to enrollees.”
2.
Investigating PBMs
Several
states have investigated or are currently investigating PBMs.
Florida:
State audit found “prescription markups” by PBMs cost Florida’s Medicaid system
$113.3 million in 2020 ($89.6 million in “spread costs”).
Kentucky: Attorney
General investigating PBMs for overcharging the state and discriminating
against independent pharmacies after state discovers PBMs kept $123.5 million
in spread annually.
Massachusetts:
Investigation found prices charged by PBMs for generic drugs were often
“markedly higher” than the actual cost of the drug in both Mass Medicaid
Managed Care and Commercial Plans, “contributing to higher health care
spending” (e.g., up to 111% more for certain drugs than in fee-for-service
state-managed Medicaid program).
Mississippi:
Auditor General is investigating PBMs suspected of overcharging state Medicaid
and the Mississippi State and School Employees’ Life and Health Insurance Plan,
which covers nearly 200,000 state employees, retirees and their families after
audit found PBMs were paid more than $1.1 billion; sometimes as much as $25
million a month.
Pennsylvania:
Auditor General found between 2013 and 2017, the amount that taxpayers paid to
PBMs for Medicaid enrollees more than doubled from $1.41 billion to $2.86
billion and is urging greater transparency and more state control.
3. Carving
out PBMs from managing Medicaid pharmacy benefits
Four
states reported in 2019 that they generally “carve out” pharmacy benefits from
their Medicaid managed care programs (Missouri, West Virginia, Tennessee
and Wisconsin) and other states were considering doing so.
West
Virginia “carved out” PBMs, including Express Scripts and CVS, from its
Medicaid managed-care program and began running the program as a
fee-for-service program – eliminating spreads and reducing administrative fees.
It expected to save $30 million a year—about 4 percent of the state Medicaid
drug spending. In fact, WV Medicaid saved $54.4 million in its first year and
$122 million that used to go to out-of-state PBMs instead went to West Virginia
pharmacies in the form of fixed dispensing fees.
Ohio
contracted with a single PBM for Medicaid after undertaking the
state audit described
above and the State Auditor concluding, “It is now overwhelmingly apparent that
PBMs are operating the biggest shell game in modern history, and we are all
paying for it.
4.
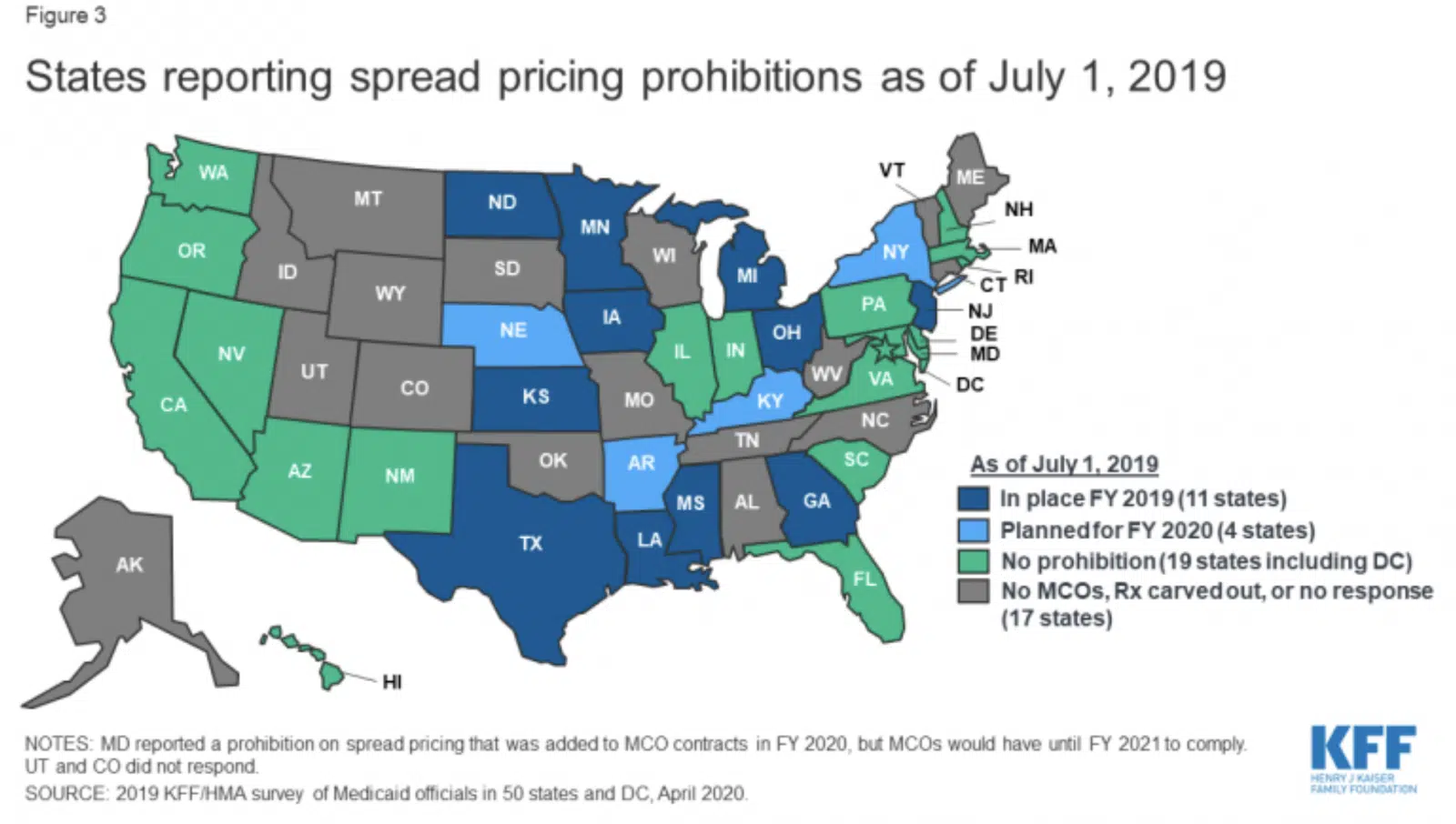
Prohibiting spread pricing
About
17 states reported a spread pricing prohibition would take effect by January
2021 (Figure 3).
Arkansas: Passed
a law, upheld by the Supreme Court, that required all PBMs to reimburse
pharmacies at a price equal to or higher than what the pharmacy paid to buy the
drug from a wholesaler.
Maryland: Banned
spread pricing after a state Medicaid report found PBMs pocketed “spread” of
$72 million annually.
Ohio: Ended
spread pricing contracts with PBMs and switched to a pass-through model
following a state audit that found PBM profit accounted for 31.4% ($208.4
million) of the $662.7 million paid by Ohio Medicaid MCOs for generic drugs
5.
Restricting PBM rebates
Ohio:
rebates and discounts must be passed back to the state.
Maine:
required PBMs to pass rebates and other “compensation” to consumers or insurers
(who must in turn apply the funds to “offset the premium for covered persons”).
West
Virginia: now handles pharmacy benefits for both state workers and Medicaid
recipients through the West Virginia State University of Pharmacy, saving $38
million in its first year.
About
17 states: have enacted stronger laws requiring PBMs to disclose rebate information.
6. Prohibiting
“claw backs”
About
38 states have prohibited PBM “claw backs.
7.
Prohibiting pharmacy discrimination
Georgia,
Louisiana, Minnesota and Utah have passed legislation banning the practice
of “pharmacy steering.”
Kentucky created
an act that requires PBMs to provide greater transparency and “fair and
reasonable” reimbursements.
8.
Restricting Section 340B reimbursements
About
11 states: have passed legislation to prohibit PBMs from reimbursing 340B
covered entities less than other entities who get their standard reimbursement
rate.
9.
Limiting “Utilization Management”
Prior
Authorization – 12 states (including RI) have legislation protecting drug
classes or categories from using Prior Authorization in some or all
circumstances, and most (excluding RI) also apply such statutory limits to
Medicaid MCOS.
Step
Therapy – 11 states have passed and many more are
considering legislation to limit Step Therapy, e.g., Arkansas became
the first state to pass a comprehensive step-therapy ban.
Non-Medical
Drug Switching – Several states have prohibited or introduced bills
limiting non-medical switching.
Potential
Roadblocks to RI Reforms
1.
CVS-Aetna-Caremark
CVS
Caremark is a large Rhode Island-based corporation whose single biggest source
of revenue is its PBM business.
Although
the full extent of corporate influence is difficult to discern, it can be
significant, and:
CVS
pays lobbyists large sums (e.g., Pharmacy Care Management Association -PCMA,
$3,962,000 in 2020) to advocate in RI against PBM reforms.
CVS
contributes to RI elected leaders who have not voted to investigate nor control
middlemen payers and PBMs as healthcare cost drivers.
CVS
has threatened to cut RI jobs to influence proposed legislation.
Since
2010, CVS has secured over $240 million in Rhode Island tax breaks despite
apparently cutting its RI workforce from about 12,000 to 3,000 (including
getting over $20 million in FY2016 and cutting 247 jobs without notice to
the state) and despite taxpayers paying for at least 300 RI CVS employees on
Medicaid.
2.
The Rhode Island Executive Office of Health and Human Services (EOHHS)
RI
EOHHS has advocated for RI Medicaid to be “managed” by private insurance
companies – despite lack of evidence that privatizing Medicaid serves consumers
and taxpayers better than the fee-for-service state-run Medicaid program
previously in place.
Today,
about 90% of RI Medicaid is run by managed care organizations (MCOs): (Neighborhood
Health Plan of Rhode Island, Tufts Health Plan and United
Healthcare Community Plan) who are paid approximately
$1.7 billion annually (about 40%
state/60% federal funds) – even though the RI Auditor General,
since 2009, has flagged inadequate state MCO oversight.
RI
MCO contracts, scheduled to expire in April 2022, are missing PBM oversight and
restrictions, e.g., they:
- do not have reporting requirements to identify the amount of PBM spread.
- do not make statutory limitations on prior authorizations also apply to Medicaid managed care PBMs.
3.
RI Office of Health Insurance Commissioner
Rhode
Island is the only state in the country to have a separate “Office of Health Insurance Commissioner”
(OHIC) whose #1 listed purpose is to “guard the solvency of health
insurers.” See RIGL §
42-14.5-2.
Although
OHIC may also seek to protect consumers, it appears to prioritize health
insurer economic interests, e.g., raising health insurance premiums during the
COVID-19 pandemic.
OHIC
recognizes prescription drug costs are major healthcare cost drivers, however,
its analyses fail to consider what role insurers and PBMs play in skyrocketing
healthcare cost.
4.
RI Health Care Costs Trends Project
The
latest major research effort to study Rhode Island healthcare costs is
the RI Health
Care Cost Trends Project (“Cost Trends Project”), a
“private-public partnership” funded by a $550,000 grant from the Peterson Center on Healthcare (PCH),
founded by Pete Peterson,
a “power from Wall Street to Washington,” who championed the theory that
“entitlement programs” like Medicare, Medicaid and Social Security, would wreck
the US economy. PCH-sponsored analyses do not analyze whether middlemen
insurers and PBMs could be cost drivers.
The
Cost Trends Project’s goals are to “identify cost and utilization drivers,
develop an annual health care cost growth target, and inform system performance
improvements.”
After
spending its initial $550,000 grant, the Cost Trends Project has produced analyses
that ignore how insurers and PBMs affect health care costs and could not
establish an accurate “annual health care cost growth target.”
A
majority of the Cost Trends Project’s steering committee and staff:
- have ties to insurance company or PBM middlemen as current or former high level employees or
- are employed by organizations that rely heavily on insurer/PBM funding; or
- have a history of producing healthcare cost analyses that fail to analyze middlemen and focus on reining in providers, despite evidence that such policies are ineffective.
What
RI Should Do
Rhode
Island legislative and executive branch officials should follow the lead of
other states more aggressively reining in PBMs, including:
- Require PBMs to disclose information that results in effective ongoing state oversight and control of PBMs.
- Pursue appropriate civil and criminal investigations and actions.
- Carve out PBMs from Medicaid Managed Care Organization (MCO) contracts set to renew in April 2022.
- Restrict Insurer/PBM middlemen unjustified revenues, such as those arising from spread pricing, “claw backs,” “pharmacy steering,” discriminatory reimbursements, manufacturer rebates, and Section 340B transactions.
- Restrict harmful Insurer/PBM utilization management practices, such as, Prior Authorization, Step Therapy and Non-medical Drug Switching.
- Establish an unbiased research group to analyze ALL potential healthcare cost drivers, including private middlemen insurers and PBMs.
WHAT
YOU CAN DO
Sign this
petition to ask state legislators, OHIC and EOHHS to reform
oversight and control over RI PBMs.
Linda L Ujifusa, Esq., Chair, RI Healthcare Access & Affordability Partnership, www.rihealthcare.org, 401-655-1446
J. Mark Ryan, MD, FACP, Chair, Physicians for a National Health Program – RI Chapter