In some anti-vaxxers, who would notice?
FIONA MACDONALD for scienceslert.com
We all know that COVID-19 can lead to lingering fatigue and brain fog. But one of the most rigorous examinations to date of the long-term cognitive impacts of severe infection has just yielded some pretty unsettling results.
In
a study comparing 46 severe COVID-19 patients with 460 matched controls,
researchers found the mental impacts of severe COVID-19 six months later can be
the equivalent to aging 20 years – going from 50 to 70 years old – or losing 10
IQ points.
The
specific mental changes were also distinct to those seen in early dementia or
general aging.
"Cognitive impairment is common to a wide range of neurological disorders, including dementia, and even routine aging, but the patterns we saw – the cognitive 'fingerprint' of COVID-19 – was distinct from all of these," says neuroscientist David Menon from the University of Cambridge in the UK, who was senior author of the study.
The
new paper doesn't set out to alarm the many of us who've already had COVID, but
instead investigate more closely how serious the cognitive changes are
following severe cases of the infection, so we can begin to understand how to
mitigate them.
"Tens
of thousands of people have been through intensive care with COVID-19 in
England alone and many more will have been very sick, but not admitted to
hospital," says lead researcher and cognitive scientist Adam Hampshire from
Imperial College London.
"This
means there are a large number of people out there still experiencing problems
with cognition many months later. We urgently need to look at what can be done
to help these people."
The
experiment involved 46 people who'd gone to Addenbrooke's Hospital in Cambridge
as a result of COVID-19 between March and July 2020. Sixteen of them were put
on mechanical ventilation during their stay.
An
average of six months after their infection, researchers supervised them using
a testing tool called Cognitron to see how they were doing in areas such as
memory, attention, reasoning, as well as anxiety, depression, and post-traumatic stress disorder.
The
researchers didn't have test results from before these individuals fell ill
with COVID to compare to. Instead they did the next best thing, and compared
their results against a matched control group of 460 people.
These
results were then mapped to see how far they deviated from expected scores for
their age and demographic, based on 66,008 members of the general public.
The
results showed that those who'd survived severe COVID were less accurate and
had slower response times than the general public.
The
magnitude of cognitive loss was similar to the effects of aging between 50 and
70 years of age – and equivalent to losing 10 IQ points.
Accuracy
in verbal analogy tasks – where people are asked to find similarities between
words – was most impacted. This mirrors anecdotal reports that suggest people
post-infection are struggling to find the right word, and feeling like their brain is in slow motion.
Interestingly,
even though patients reported varying levels of fatigue and depression, the
severity of the initial infection, rather than the survivor's current mental
health, could best predict the cognitive outcome, the team found.
"These
results indicate that although both fatigue and mental health are prominent
chronic [consequences] of COVID-19, their severity is likely to be somewhat
independent from the observed cognitive deficits," the researchers write in their paper.
The
somewhat good news is that, upon follow up, there were some signs of recovery –
but it was gradual at best.
"We
followed some patients up as late as ten months after their acute infection, so
were able to see a very slow improvement," says Menon.
"While
this was not statistically significant, it is at least heading in the right
direction, but it is very possible that some of these individuals will never
fully recover."
This
study only looked at the more extreme end of hospitalized patients, but there
are plenty of other studies showing that even 'mild' cases can cause similar cognitive impacts.
What's
still not fully understood is why and how the SARS-CoV-2 virus causes this cognitive decline.
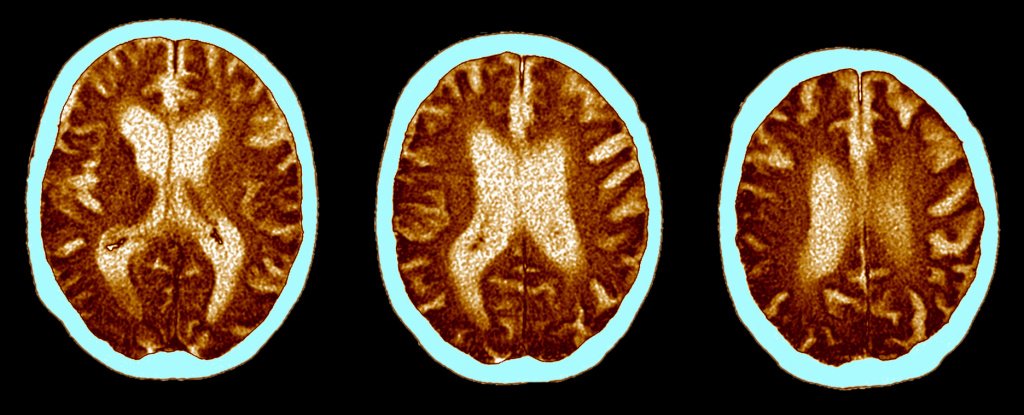
Previous
research has shown that during severe COVID, the brain decreases
glucose consumption in the frontoparietal
network, which is involved in attention, problem solving, and
working memory. It's also known that the virus can directly affect the
brain.
But
the researchers suggest the likely culprit isn't direct
infection, but a combination of factors: including reduced oxygen or blood supply to the brain; clotting of vessels; and
microscopic bleeds.
There's
also mounting evidence that the body's own immune and inflammatory response may be having a significant
impact on the brain.
"Future
work will be focused on mapping these cognitive deficits to underlying neural
pathologies and inflammatory biomarkers, and to longitudinally track recovery
into the chronic phase," the researchers write.
Until
then, take comfort in the fact that if you're still feeling slow and foggy
months after recovering from COVID-19, you are most certainly not alone.
The
research has been published in eClinical Medicine.