Brown scholars offer key facts and insights on the persisting public health emergency.
Brown University
Even before the U.S. had emerged from the COVID-19 pandemic, the country’s first case of the monkeypox virus was reported in May 2022. In late July, the World Health Organization declared the ongoing monkeypox outbreak a public health emergency, and in early August, the U.S. government followed suit.
Over
the past few months, the monkeypox outbreak has both offered opportunities to
apply lessons learned from COVID and presented its own unique challenges.
Although the U.S. is currently seeing a decline in cases, the outbreak continues
to affect patients both domestically and abroad.
Scholars
from Brown’s School of Public Health and Warren Alpert Medical School offered
some key facts and insights on this complicated public health issue.
Philip A. Chan
Associate
professor of medicine, associate professor of behavioral and social sciences;
consultant medical director of the Rhode Island Department of Health
Gay, bisexual and other men who have sex with men are primarily being affected by monkeypox —although anyone can get it.
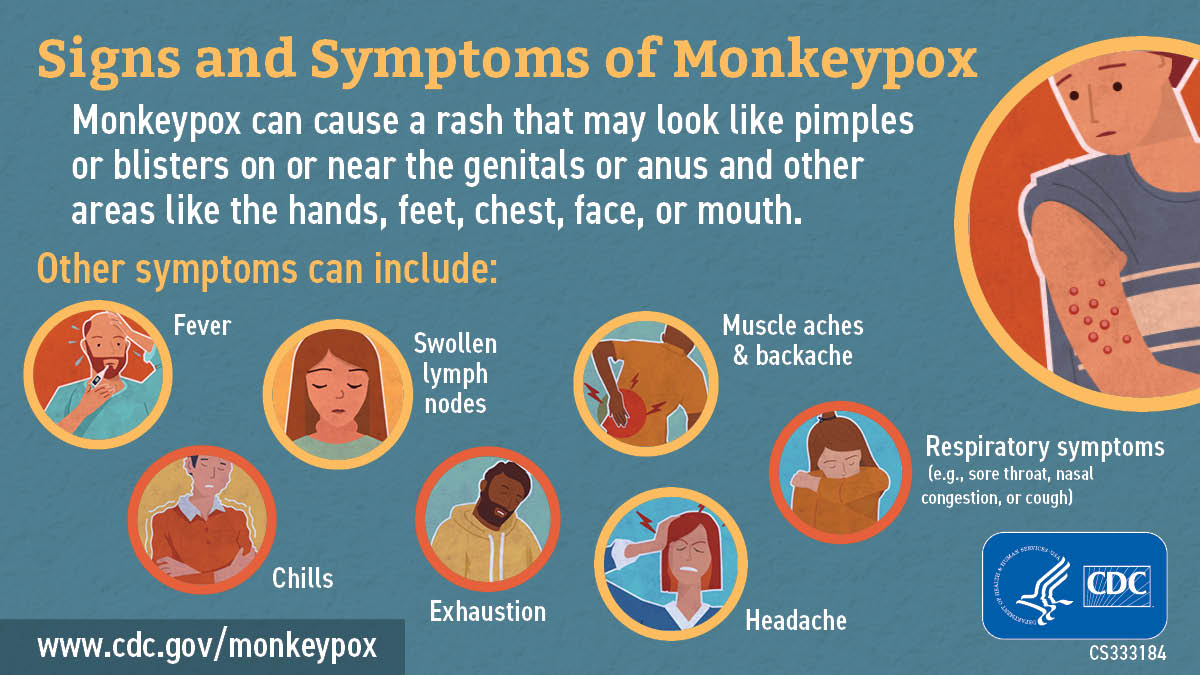
The
virus can spread via direct contact with a person with monkeypox or by touching
objects, fabrics and surfaces that have been used by someone with monkeypox. We
don't know yet whether monkeypox is sexually transmitted, but it is associated
with sex. It was initially believed that monkeypox was spreading by droplets
(similar to SARS-CoV-2), but that type of transmission appears to be much less
common than expected. Monkeypox is much less infectious than COVID-19.
Gay,
bisexual and other men who have sex with men are primarily being affected by
monkeypox — although anyone can get it. It is important for public health to
continue to actively communicate risk to affected populations so they can make
informed decisions about behavioral changes and prevention options, which
include vaccination.
Despite
the death of a person in the U.S. from monkeypox (and
a second possible death in Texas under investigation), it is not believed that
the virus is becoming more lethal. We do know that people who are immunocompromised
(e.g., who are HIV-positive with a low CD4 cell count), who are receiving
chemotherapy, or who have been diagnosed with certain other medical conditions)
are at higher risk of complications from monkeypox. People who are
immunocompromised and diagnosed with monkeypox should seek treatment
immediately.
There
is a need for more federal public health resources to address monkeypox, as
well as COVID-19, avian flu and whatever else happens in the future. Our
country is in urgent need of a framework and a national plan with resources on
how to address these emerging threats to public health.
Joseph
Metmowlee Garland
Associate
professor of medicine, clinician educator; medical director, Infectious
Diseases and Immunology Center, the Miriam Hospital
Unfortunately, you can’t just get a monkeypox vaccine at your local pharmacy like you can the COVID vaccines.
The
monkeypox vaccine is issued from the CDC directly to state health departments,
who determine how to distribute their limited supply to the highest-risk
populations. Unfortunately, you can’t just get a monkeypox vaccine at your
local pharmacy like you can the COVID vaccines.
On
top of that, there’s a shortage, which is the result of several factors. First,
the vaccine is intended for smallpox, so those planning for a stockpile were
not necessarily anticipating a widespread outbreak of monkeypox. Further,
expiring vaccines had not been not replenished and there were delays in
ordering and securing replacement vaccines. The vaccine we are using, Jynneos,
involves two doses; it is only manufactured by one company in Denmark, and they
have a certain capacity. The global spread of this epidemic has put an acute
demand on the vaccine manufacturers from countries around the world, including
many in Europe.
In
order to get the vaccine to more people, providers are following the CDC’s alternative dosing regimen of
administering the vaccine intradermally, or between the skin layers, instead of
subcutaneously, or under the skin. An intradermal vaccine can induce a stronger
immune response because of how many immune cells we have in our skin. The FDA
did a study on the difference between intradermal and subcutaneous
administration of the Jynneos vaccine at the currently used doses and found
that study participants had similar levels of immune response (measured by
antibody levels) with the lower dose intradermal vaccine. That allows us to give
a much lower dose to get the same level of effect: one-fifth of the dose
induces the same level of immune response in studies — that allows for
potentially five times as many people to get the vaccine.
But
there’s a trade-off. In general, this is a harder way to administer a vaccine,
and more people have skin reactions to this method— we’ve seen mild swelling,
redness or discoloration at the injection site. In some people, that can
persist for a long time, which is important to be aware of.
And
it must be said that no vaccine is 100% effective. We don’t have much data on
any vaccines for monkeypox specifically. Jynneos was tested in an animal model
of smallpox (a very similar and related virus), but we still need to see actual
results in a real-world setting. Data show that it takes about six weeks from
the first dose (and two weeks after the second dose) for people to reach full
immunity. Up until that time, people still have a risk of being infected. After
that time, most people should have protective immunity — but again, we still
will need to back that up with real-world data as we accumulate it.
Amy
S. Nunn
Professor
of behavioral and social sciences, professor of medicine; executive director,
Open Door Health
We haven’t encountered much vaccine hesitancy with monkeypox at Open Door Health. Our challenge has been unprecedented demand for a new service.
At
our Open Door Health clinic, we provide primary
care and other preventative and sexual health services for the LGBTQ+
population. We have vaccinated over 700 people to date, and more people are
coming in every day.
We
always ask the people we serve what they want, and how we can do it in the way
that’s best for them — instead of telling them what we think is best for them.
One thing that came up in our community listening tour with gay men was that
people were worried about scarring on their face, body or genitalia, and they
said that concerns about scarring really motivated them to get vaccinated.
People were also afraid of getting sick, or experiencing a great deal of pain
from monkeypox.. People were also afraid of getting sick or experiencing pain
caused by monkeypox.
We
haven’t encountered much vaccine hesitancy with monkeypox at Open Door Health.
Our challenge has been unprecedented demand for a new service.
We
built the infrastructure to do this very fast. When we started, the entire
clinical team worked 80-hour weeks so that we could offer the monkeypox vaccine
to everyone who walked through the clinic’s doors – men who have sex with men,
sex workers and others who might be at risk. Now we’re trying to integrate
monkeypox vaccinations into our primary care work flow. The thing is, there’s
currently no federal funding for this work that we can access. We do it because
it’s important to the people we serve and aligns with the clinic’s mission and
values, but this mission has cost the clinic $200,000 so far in terms of staff,
time, communications – we’ve even had to bump other priorities. There needs to
be a federal financial response to the monkeypox outbreak to help clinics like
ours care for our patients. This problem isn’t unique to us; this is a crisis
for clinics around the country who want to do the right thing.
William
C. Goedel
Assistant
professor of epidemiology
To
keep on top of the monkeypox outbreak, we need to accelerate access to
promising therapeutics.
For most people with monkeypox, treatment generally involves symptom management. But the antiviral drug Tecovirimat (also known as TPOXX) may be able to alleviate severe symptoms. TPOXX is approved by the U.S. Food and Drug Administration for the treatment of smallpox, a virus similar to monkeypox. Health care providers can request TPOXX through their local health department, but they may be unaware of its availability or the process for obtaining it. Because TPOXX was developed to work against smallpox as part of a bioweapons strategy in response to the events of 9/11, TPOXX is only available from the Strategic National Stockpile. In order to prescribe it, providers are required to fill out significant amounts of paperwork. This process creates a barrier to access: The bureaucratic process for obtaining tecovirimat from the CDC is cumbersome and time-consuming for providers.
To
keep on top of the monkeypox outbreak, we need to accelerate access to
promising therapeutics. The development of an emergency use protocol by the CDC
could significantly streamline the process, saving precious time for patients
in need of the medication. In the meantime, it’s essential that
prescribers are trained and educated about this monkeypox treatment — not just
how to use it, but the steps to obtain it from the CDC and the paperwork
involve in that process.
Jennifer
Nuzzo
Professor
of epidemiology; inaugural director of the Pandemic Center at the Brown
University School of Public Health
We
need to learn from this to move forward with this outbreak and future
pandemics… And we need to train future public health leaders to act swiftly in
the face of a new infectious disease threat.
JENNIFER NUZZO Professor of epidemiology; inaugural director of the Pandemic Center at the Brown University School of Public Health
The outbreak of monkeypox in the U.S. was yet another test of our country's capacity to act swiftly and effectively to stop the spread of an emerging pathogen. We were well-positioned to succeed. Public health labs in states throughout the country and at the CDC had the capacity to run tests for the virus when it was first detected. The U.S. had a stockpile of vaccines to stop transmission and experimental treatments to heal patients. However, we were slow to expand use of these tools and to make sure that patients and health care providers could access them easily enough to rapidly stop the virus from becoming entrenched.
We also lacked the ability to rapidly assemble and
analyze data on who was getting monkeypox and to ensure that our efforts to
expand testing, vaccinate and offer treatments were sufficient or whether we
needed to change course. And we struggled to communicate who was likely
most at risk of infection and how they can protect themselves without encouraging
stigmatization of these patients. These missteps allowed the virus to spread
throughout the U.S. and jeopardize prospects for containment.
We
need to learn from this to move forward with this outbreak and future
pandemics. Infectious disease threats — like monkeypox, COVID-19 and the recent
resurgence of polio — are the hazards of our time, and we need to prepare for
them as we would for other recurring hazards, like natural disasters, fires or
hurricanes. We need to build better data systems and a well-coordinated,
responsive testing system that can identify cases early, accurately and
efficiently. And we need to train future public health leaders to act swiftly
in the face of a new infectious disease threat, even when there is uncertainty
about how it may unfold.