Marta Gaglia, Tufts University and Seema Lakdawala, University of Pittsburgh
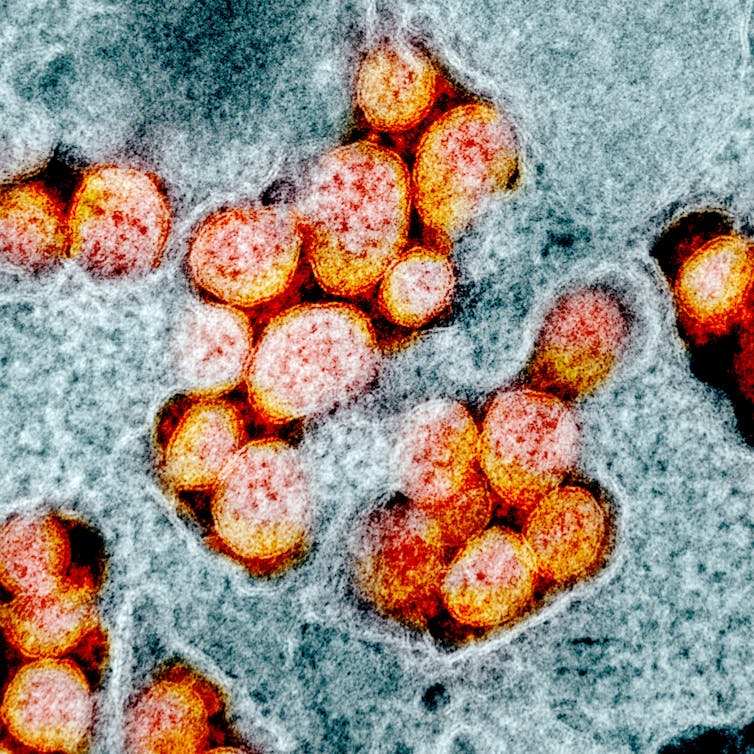 |
| SARS-CoV-2 virus particles, isolated from a patient and imaged using a transmission electron micrograph. NIAID |
Two basic virological concepts have gotten a lot of attention recently – the “infectious dose” and the “viral load” of SARS-CoV-2.
As influenza virologists, these are concepts that we often think about when studying respiratory virus infections and transmission.
What is an ‘infectious dose’?
The infectious dose is the amount of virus needed to establish an infection.
Depending on the virus, people need to be exposed to as little as 10 virus particles – for example, for influenza viruses – or as many as thousands for other human viruses to get infected.
Scientists do not know how many virus particles of SARS-CoV-2 are needed to trigger infection.
COVID-19 is clearly very contagious, but this may be because few particles are needed for infection (the infectious dose is low), or because infected people release a lot of virus in their environment.
EDITOR'S NOTE: To me, this would really help on issues such as touching things (e.g. deliveries or groceries). Studies have shown the COVID-19 virus can dwell on surfaces for hours if not days, BUT the actual amount of the virus on that surface falls off dramatically and very quickly (see charts, below). The authors are saying that science doesn't have enough information to say whether or not that matters. - W. Collette

What is the ‘viral load’?
The viral load is the amount of a specific virus in a test sample taken from a patient. For COVID-19, that means how many viral genomes are detected in a nasopharyngeal swab from the patient.
The viral load reflects how well a virus is replicating in an infected person. A high viral load for SARS-CoV2 detected in a patient swab means a large number of coronavirus particles are present in the patient.
Is a high viral load linked to higher risk of severe pneumonia or death?
Intuitively it might make sense to say the more virus, the worse the disease. But in reality the situation is more complicated.
In the case of the original SARS or influenza, whether a person develops mild symptoms or pneumonia depends not only on how much virus is in their lungs, but also on their immune response and their overall health.
Right now it is unclear whether the SARS-CoV-2 viral load can tell us who will get severe pneumonia.
Two studies in The Lancet reported people who develop more severe pneumonia tend to have, on average, higher viral loads when they are first admitted to the hospital.
These studies also reported that the viral loads remain higher for more days in patients with more severe disease. However, the difference was not dramatic, and people with similar viral loads went on to develop both mild and severe disease.
Complicating the picture further, other studies found that some asymptomatic patients had similar viral loads to patients with COVID-19 symptoms. This means that the viral load alone is not a clear predictor of disease outcome.
Another common question is whether getting a higher virus dose upon infection – for example, through prolonged exposure to an infected person, like health care workers’ experience – will result in more severe disease.
Right now, we simply do not know whether this is the case.
Does high viral load increase ability to pass the virus to others?
In general, the more virus you have in your airways, the more you will release when you exhale or cough, although there is a lot of person-to-person variation. Multiple studies have reported that patients have the highest viral load of the coronavirus at the time they are diagnosed.
This means that patients transmit COVID-19 more effectively at the beginning of their illness, or even before they know they are sick.
This is bad news.
It means people who look and feel healthy can transmit the virus to others.
Why is it hard to answer basic questions about virus amounts for SARS-CoV-2?
Normally, researchers like us determine the characteristics of a virus from a combination of highly controlled experimental studies in animal models and epidemiological observations from patients.
But since SARS-CoV-2 is a new virus, the research community is only just beginning to do controlled experiments.
Therefore, all the information we have comes from observing patients who were all infected in different ways, have different underlying health conditions, and are of different ages and both sexes.
This diversity makes it difficult to make strong conclusions that will apply to everyone from only observational data.
Where does the uncertainty on viral loads and infectious dose leave us?
Studying viral loads and the infectious dose will likely be important to make better decisions for health care providers.
For the rest of us, regardless of the viral load of patients or the SARS-CoV-2 infectious dose, it is best to reduce exposure to any amount of virus, since it is clear the virus is transmitted efficiently from person to person.
Current social distancing practices and limited contact with groups of people in enclosed spaces will reduce the transmission of SARS-CoV-2.
In addition, the use of face masks will reduce the amount of virus released from presymptomatic and asymptomatic individuals. So stay home and stay safe.
[Get facts about coronavirus and the latest research. Sign up for The Conversation’s newsletter.]
Marta Gaglia, Assistant Professor of Molecular Biology & Microbiology, Tufts University and Seema Lakdawala, Assisstant Professor, University of Pittsburgh
This article is republished from The Conversation under a Creative Commons license. Read the original article.