Complications Include Stroke, Hemorrhage, and more
By RADIOLOGICAL SOCIETY OF NORTH AMERICA
The largest multi-institutional international study to date on brain complications of COVID-19 has found that approximately one in 100 patients hospitalized with COVID-19 will likely develop complications of the central nervous system.
These can include stroke, hemorrhage, and other potentially fatal complications. The study is being presented at the annual meeting of the Radiological Society of North America (RSNA).
“Much has been written about the overall pulmonary problems related to COVID-19, but we do not often talk about the other organs that can be affected,” said study lead author Scott H. Faro, M.D., FASFNR, professor of radiology and neurology and director of the Division of Neuroradiology/Head & Neck Imaging at Thomas Jefferson University in Philadelphia.
“Our study
shows that central nervous system complications represent a significant cause
of morbidity and mortality in this devastating pandemic.”
Dr. Faro initiated the study after discovering that existing literature on central nervous system complications in hospitalized COVID-19 infected patients was based on a relatively small number of cases.
To derive a more complete picture, he and his colleagues analyzed
nearly 40,000 cases of hospitalized COVID-19 positive patients from seven U.S.
and four western European university hospitals. The patients had been admitted
between September 2019 and June 2020. Their average age was 66 years old, and
there were twice as many men as women.
 |
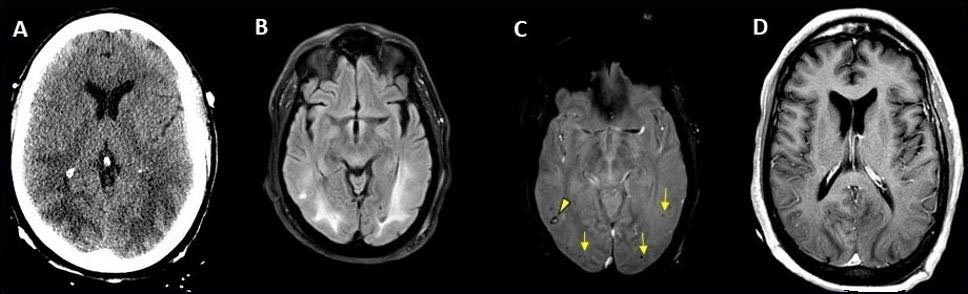
| Hemorrhage seen in 56-year-old female with COVID-19 infection and no other significant past medical history. Credit: RSNA and Scott H. Faro, M.D. |
The most common cause of admission was confusion and altered mental status, followed by fever. Many of the patients had comorbidities like hypertension, cardiac disease, and diabetes.
There were 442 acute neuroimaging findings that were most likely
associated with the viral infection. The overall incidence of central nervous
system complications in this large patient group was 1.2%.
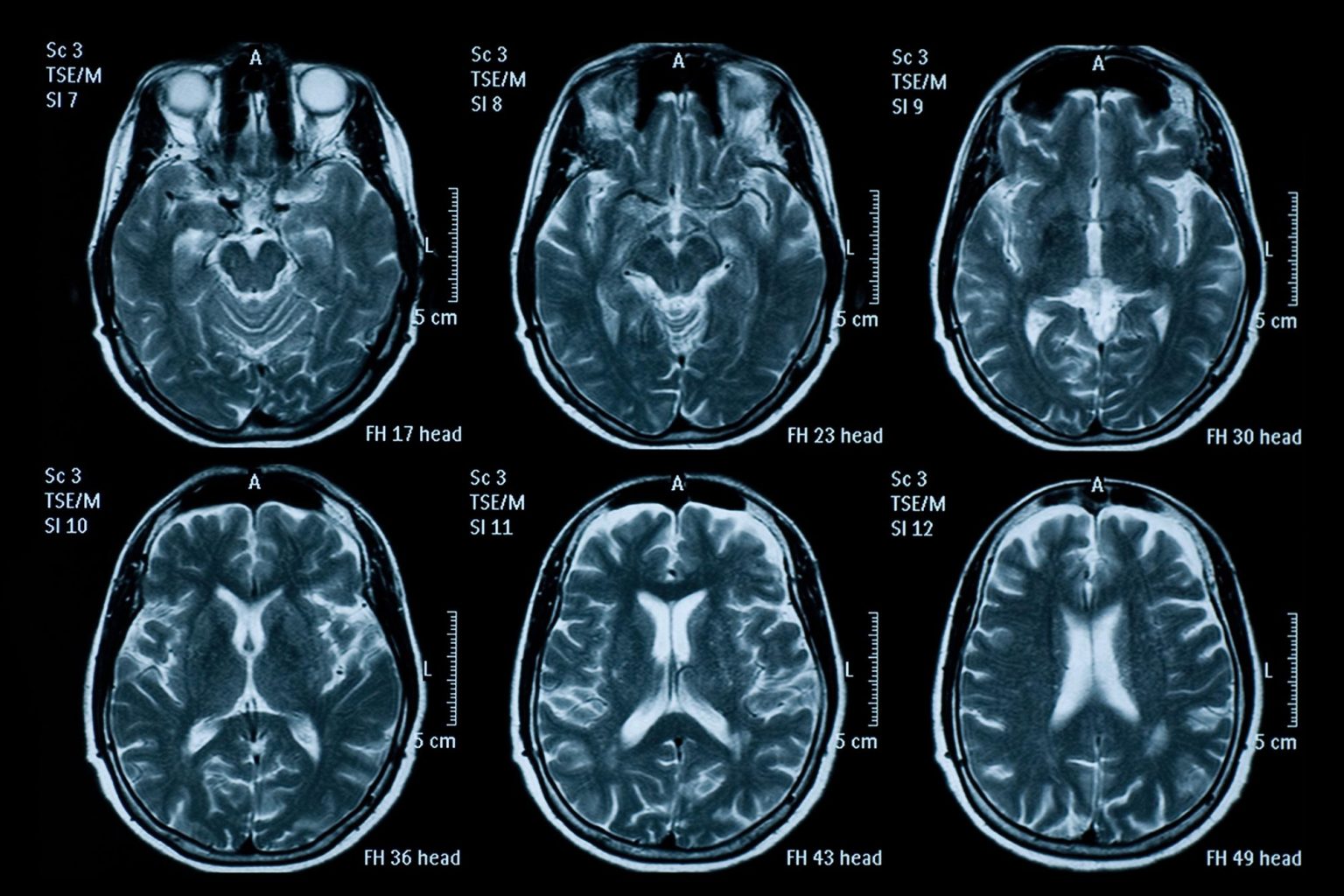
“Of all the inpatients who had imaging such as MRI or a CT scan of brain, the exam was positive approximately 10% of the time,” Dr. Faro said. “The incidence of 1.2% means that a little more than one in 100 patients admitted to the hospital with COVID-19 are going to have a brain problem of some sort.”
The most common complication was ischemic stroke, with an incidence of 6.2%, followed by intracranial hemorrhage (3.72%) and encephalitis (0.47%), an inflammation of the brain.
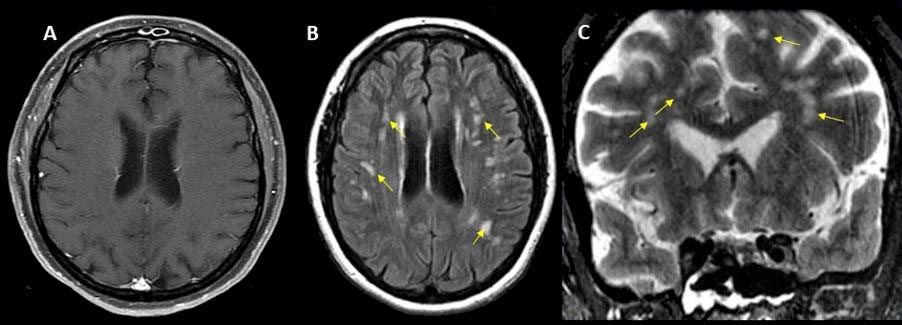
The researchers also discovered a small percentage of unusual
findings, such as acute disseminating encephalomyelitis, an inflammation of the
brain and spinal cord, and posterior reversible encephalopathy syndrome, a
syndrome that mimics many of the symptoms of a stroke.
“It is important to know an accurate incidence of all the major
central nervous system complications,” Dr. Faro said. “There should probably be
a low threshold to order brain imaging for patients with COVID-19.”