Looking for prevention for this intestinal scourge
Kate Schweitzer1, JAMA
Medical News
This past winter, cases of norovirus, a highly contagious stomach bug characterized by sudden vomiting and diarrhea, surged in the US. Nicknamed the “Ferrari of viruses” for how fast it spreads, it’s also known for racing through cruise ships, long-term care facilities, and school cafeterias. But, according to those who study it, the virus hasn’t gotten the attention it deserves.
The virus is a leading cause of
acute gastroenteritis worldwide. In the US, it causes more than 50% of
all foodborne illnesses. And each year it accounts for nearly half a million
emergency department visits, mostly for young children, and roughly 900 deaths,
predominantly in older adults, according to the US Centers for Disease Control
and Prevention.
In well-resourced regions, norovirus
symptoms commonly pass after a few extremely unpleasant days, but
“there are other places on the planet where diarrhea really does threaten the
health of populations, especially those already suffering from malnutrition,
chronic starvation, or dehydration,” said C. Buddy Creech, MD, MPH, director of
the Vanderbilt Vaccine Research Program at Vanderbilt University Medical
Center. “It’s a significant driver of mortality around the globe.”
Norovirus contributes
to nearly 1 in 5 episodes of diarrheal disease worldwide and causes
about 200 000 deaths
annually. The most vulnerable populations include children younger than 5
years, older adults, and people who are immunocompromised. In developing
countries, deaths from norovirus are common among children—who make up more than a third of the global death toll.
Preventive measures like improved water, sanitation, and hygiene have not proved effective enough to control the notably transmissible virus, which incurs a $60 billion cost to society—including $4.2 billion in health care costs—globally every year.
It’s for these reasons that the World Health Organization called developing a vaccine for it a priority in 2016. Since then, vaccine developers have struggled to create a safe and effective option. Currently, a handful of candidates are in various stages of clinical trials, including one that would be offered in the form of an oral tablet—a promising approach for a virus with such a devastating grip on resource-limited nations.
“No one is developing a norovirus vaccine in order to avoid
the occasional cruise ship outbreak,” said Creech, who is also the Edie Carell
Johnson chair and professor of pediatric infectious diseases at Vanderbilt.
“We’re doing it so we can protect the world’s most vulnerable from potentially
devastating illness.”
Why Norovirus Is So Tricky
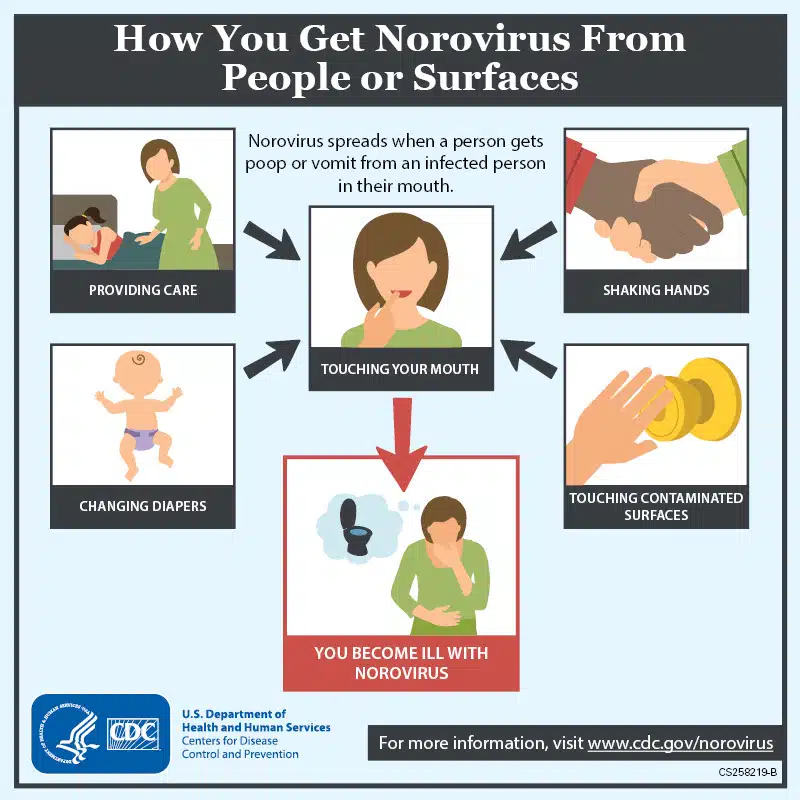
What makes the norovirus “incredibly tricky” to manage is,
in part, how it’s spread, said William Schaffner, MD, a professor of preventive
medicine and infectious diseases at the Vanderbilt University Medical Center.
“It’s not just touching and then ingesting from contaminated
surfaces,” he said. “It can also spread through the air. You can actually
inhale the virus, and just a trace of it is enough.” Not only that, people who
have recovered from the infection can continue to shed the virus for weeks, and
it can live on surfaces for even longer.
In addition to its most noteworthy adverse effects,
norovirus infection can also cause fever and headaches, which is why Schaffner
said it’s often referred to as a stomach flu despite being unrelated to
influenza.
Variability in the severity of norovirus illness adds to the
complexity. As Creech noted, the “disease burden is a U-shaped curve” in terms
of demographic risk.
“Most people recover, but the very young and those older,
frail people are the ones who run into trouble and end up in the hospital to
get rehydrated,” Schaffner said.
These factors make norovirus a “perfect pathogen,” noted
Lisa Lindesmith, MS, a senior scientist who is studying the virus at the
University of North Carolina at Chapel Hill. “It’s highly infectious, it’s very
environmentally stable, and there’s a tremendous amount of diversity within the
family.”
But a perfect pathogen makes for a challenging task, rife
with scientific barriers, for vaccine developers.
Based on genetic differences, researchers have divided
noroviruses into nearly 50 genotypes split into 10 groups. Five of these
groups are known to infect people, with genotype I (GI) and GII being most
common. Similar to influenza virus, dominant norovirus strains change and evade
immune systems. GII.17
caused most of the norovirus cases in the US this past winter, when
there were 2630 outbreaks—nearly double those of the previous year.
Meanwhile, GII.4, known as Sydney, has
been the most prevalent strain for more than a decade and the one associated
with the most severe illness.
“These GII.4 viruses are the ones that cause pandemic levels
of disease and cyclical patterns over time,” Lindesmith said. “They are
particularly good at changing themselves, which leads to evasion of the
immunity that you’ve already developed. When you think about young children who
have the most severe disease, it’s easy to see what a challenge this is. We’ve
got an immature immune system that’s going to need to build through repeat
exposure, yet we have a virus that’s continually changing.”
On top of that, researchers don’t know how long immunity
lasts after a norovirus infection—depending on the study, estimates range
from several months to up to 9 years. And human norovirus cultivation has not
been possible until
recently: “It’s rather difficult to grow it in laboratory conditions, so
that’s caused delays in development as well,” Schaffner said of vaccine
research.
The Challenges Facing Norovirus Vaccine Makers
Scientists have taken several different approaches toward a
norovirus vaccine, but all have progressed in fits and starts.
One of the most advanced vaccine candidates contains
viruslike particles (VLPs), empty structures that imitate the size and shape of
the pathogen but lack its genetic material. “It looks just like the virus to
your immune system, so, in theory, you can make the appropriate response
without being exposed to the replicating virus,” Lindesmith said of this
vaccine technology, which has so far been used to protect against human
papillomaviruses and hepatitis B and E. Developers have posted positive efficacy and immunogenicity data
for the investigational VLP norovirus vaccine in adults but the same candidate
failed to protect infants in a trial, manufacturer HilleVax announced in
July 2024.
Moderna, which has also been at the forefront of norovirus
vaccine development with its single-dose messenger RNA–based candidate,
mRNA-1403, had its own setback, the pharmaceutical company announced in
February. The US Food and Drug Administration (FDA) put a temporary hold on a
phase 3 clinical trial of mRNA-1403 following a single reported case of
neurological disorder Guillain-Barré syndrome. The trial launched in September
2024 with a recruitment goal of 25 000
participants globally.
Moderna did not respond to a request by JAMA Medical News
for comment, but noted in its press release that an investigation was under way
and that it “does not expect an impact on the study’s efficacy readout
timeline.”
Another platform, live-attenuated vaccines, has been
successful for rotavirus and influenza, but Lindesmith said it’s not currently
possible to grow the norovirus at the scale necessary for this. Still, new
discoveries may make this possible in the future. Over almost a decade of work,
scientists have made significant advances in
norovirus cultivation, and in January, researchers from Baylor College of
Medicine in Houston showed that they were able to reliably grow the virus in a
“mini gut,” an
organoid culture system that mimics human intestines.
Another novel approach involves piggybacking on the highly
effective vaccines for rotavirus, an unrelated pathogen that also causes
diarrhea. Researchers engineered an
experimental combination vaccine by adding a key protein from
norovirus to a harmless strain of rotavirus, and it induced the production of
neutralizing antibodies against both. The results, while encouraging, were from
preclinical studies of mice—which are not representative of human norovirus
infection—and the researchers still need to demonstrate that the immunized
animals are less likely to get sick from norovirus before it can move forward
as a solution for broad-spectrum protection.
The Potential for a Norovirus Pill
Most recently, a biotech company has sought to bring a
norovirus vaccine to market with a pill. Administered orally in a coated tablet
form, Vaxart’s delivery platform is an adenovirus
vector vaccine designed to stimulate mucosal immunity, which could be
the key to preventing norovirus infections at their starting point, said Becca
Flitter, PhD, MPH, director of immunology at Vaxart, which also has an oral
influenza vaccine in development.
In May, researchers published
promising data on the pill from a trial during which participants were
intentionally exposed to the virus.
“Unlike a large trial with 30 000
people where we only see who gets disease and who doesn’t, a
challenge study like this one allows scientists to get blood samples and even
stool samples in the hours or days before symptoms occur, so they get to know a
lot more about the actual cadence and rhythm of the response to the vaccine,” Creech said.
Half of the nearly 150 participants, aged 18 to 49 years,
received the oral vaccine, and a month later, all participants ingested the
GI.1 strain of norovirus in a liquid dose “hard enough” to ensure people got
infected, Flitter noted.
By the following week, 82% of the placebo group was infected
compared with 57% of the vaccinated group, a 30% relative reduction.
Additionally, Flitter and her coauthors found that those who received the
vaccine shed less virus in their stool and vomit than those who got the
placebo, suggesting the vaccine could slow the spread of the virus.
The reduction in the severity of disease symptoms, however,
was not
statistically significant. Flitter said this may be due, in part, to the
fact that participants received higher amounts of virus than they’d encounter
in real-world settings.
This phase 2 proof-of-concept study, which appeared in Science
Translational Medicine, followed previous analyses that found the
tablet induced mucosal
immunity in older adults and broadly
neutralizing antibodies against norovirus. In a press
release, Vaxart also announced results of a trial focused on breastfeeding
mothers: it showed an increase in norovirus antibodies in their breastmilk,
which suggests the potential for passive transfer to infants.
Lindesmith, who coauthored two of the studies on the oral
pill with Flitter, acknowledged that the strain they tested, GI.1, isn’t
responsible for the bulk of global infections. “We really have the
epidemiological data to support this need for GII.4 to be the target as a
matter of public health,” she said.
In June, Vaxart reported in a press
release that a second-generation version of the vaccine protected
against both GI and GII viruses in a phase 1 trial and, according to Flitter,
the candidate has “greater potency and enhanced immunogenicity in humans.”
Flitter said she’s excited about the possibility of “forging
a new path” with the tablet format.
“With a pill, you don’t need the infrastructure you need
with a needle,” she said. “You don’t need trained professionals who know how to
inject. You can keep it at room temperature, so bags of pills could be shipped
to wherever there’s a need, with no medical waste.”
This will work well with the at-risk older adult population,
but not the other side of that U curve, Creech noted. “My anticipation is that
we start with an oral tablet and move into a liquid formulation, like we do
with oral rotavirus vaccine, that can be given to [infants and] younger
children,” he said, adding that this will take time. “Hopefully through
vaccinating adults first, we can start to reduce the likelihood of transmission
to those who are most vulnerable who cannot yet be vaccinated.”
Of course, without an approved vaccine, these considerations
are still a long way off. Vaxart has yet to begin a phase 3 trial of its oral
pill. Flitter is currently prepping phase 2b trials for the second-generation
version.
Lindesmith acknowledges the challenges that still lie ahead.
She said the field is “not just solving for the GII.4 of today but also the
GII.4 of tomorrow” and estimates the earliest possible approval for any
norovirus vaccine is still years away. Creech predicts that an application to
the FDA is 5 years out.
Even then, most experts predict that, due to norovirus’s
rapid evolution, a vaccine will function much like flu shots and require
regular boosters. But “something is better than nothing,” Schaffner said.
“If it’s not preventing the virus altogether, we want to see
the disease blunted at the very least,” said Creech, who suggested
administering it in anticipation
of an outbreak or in advance of travel. “Driving down the burden of
this illness has tremendous societal benefit.”
Article Information
Published Online: July 25, 2025.
doi:10.1001/jama.2025.10673
Conflict of Interest Disclosures: Dr Creech
reported receiving grant support from the National Institutes of Health, the US
Centers for Disease Control and Prevention, and Moderna and serving as a
consultant for Sanofi, Merck, TDCowen, Guidepoint Global, Delbiopharm, and
Dianthus. He also reported serving on the data and safety monitoring board for
GSK and Bavarian Nordic. Ms Lindesmith reported holding patents on norovirus
vaccine and therapeutics designs, including coinventorship with Vaxart. She
also reported ongoing collaborations with HilleVax, GIVAX, Vaxart, Merck, and
Maine Biotech related to norovirus vaccines, therapeutics, and diagnostics and
that she has served as an external consultant for HilleVax and Merck. Dr
Flitter reported owning stock options in Vaxart and that funding for all
clinical trials she authored was from Vaxart except for the maternal breastmilk
study conducted in South Africa, which was partially funded by the Gates
Foundation. No other disclosures were reported.